is self-mutilation a symptom od dementia
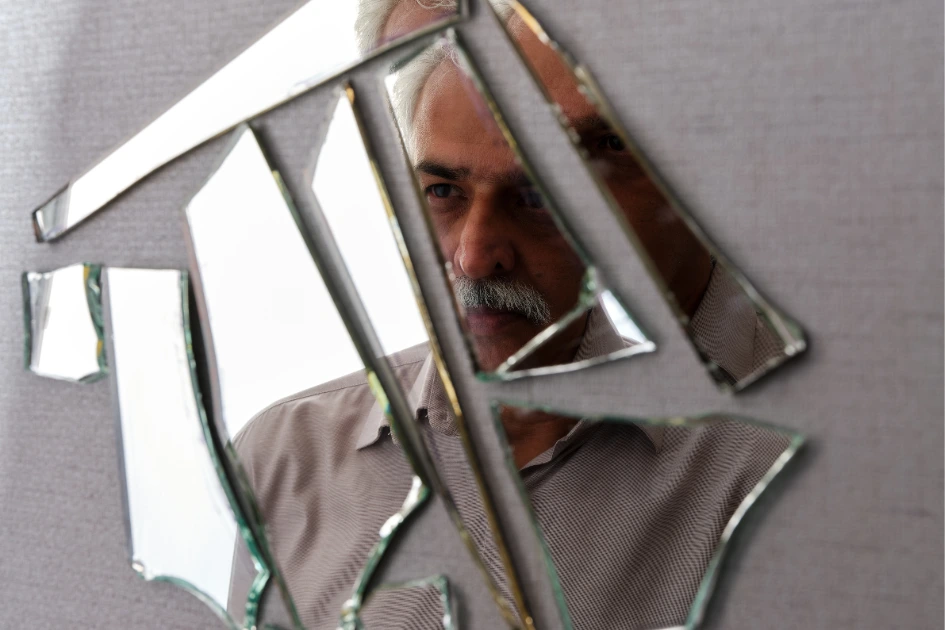
Is self-mutilation a symptom od dementia? “It started with small bruises, things she said were accidents. But deep down, you knew something was changing.”
Is self-mutilation a symptom of dementia? If you’re here, chances are you’ve witnessed something unsettling, perhaps repeated injuries on a parent or partner with dementia, or behaviors that suggest they’re intentionally hurting themselves. It’s a frightening moment when you realize these aren’t isolated incidents. You start asking painful questions: Is this happening? Could self-mutilation be a symptom of dementia? What does this mean for their care?.
You’re not overreacting. Recognizing these signs is the first critical step toward protecting someone you love. While dementia is widely known for memory loss and cognitive decline, the emotional and behavioral shifts can be just as profound and sometimes far more difficult to understand. In some cases, individuals with dementia may engage in self-harm behaviors, not out of a desire to end their life, but as a distorted response to confusion, discomfort, or unmet emotional needs.
In this comprehensive guide, you’ll explore the complex link between dementia and self-injury, gain insight into the reasons behind these behaviors, and learn how to respond appropriately. Whether you’re looking for immediate safety strategies, long-term care plans, or information about self-harm treatment centers and self-harm scar treatment, you’ll find guidance grounded in compassion and backed by clinical insight.
Healthy Family Relationships: How do you know you are in a healthy relationship with your family?
You are not alone in this journey, and the more you understand, the more empowered you become to provide the care they need.
Table of Contents
Understanding Dementia and Behavioral Changes
When trying to understand unusual or harmful behaviors in someone with cognitive decline, it’s essential to begin with the basics. Dementia isn’t just about forgetfulness; it’s a complex neurological syndrome that gradually affects how a person thinks, behaves, and interacts with the world around them. These shifts can be disorienting for both the individual and those who care for them.

What Is Dementia?
Dementia is not a single disease but a general term used to describe a range of cognitive disorders that interfere with daily life. It’s caused by damage to brain cells, which impacts their ability to communicate with one another. As a result, thought processes, memory, emotions, and even physical coordination may deteriorate over time.
There are several types of dementia, each with unique patterns of decline:
- Alzheimer’s Disease: The most common form, marked by gradual memory loss and disorientation.
- Lewy Body Dementia: Often involves visual hallucinations, sleep disturbances, and fluctuating attention.
- Frontotemporal Dementia (FTD): Typically causes personality changes, impulsivity, and poor judgment.
- Vascular Dementia: Related to reduced blood flow to the brain, often following a stroke or series of mini-strokes.
Each type of dementia brings its own set of challenges, but most share some common symptoms:
- Memory loss that disrupts daily life
- Difficulty communicating or finding words
- Impaired judgment and decision-making
- Emotional volatility or apathy
- Repetitive or compulsive behaviors
These behavioral symptoms are key to understanding why you might wonder, Is self-mutilation a symptom of dementia? As dementia progresses, some individuals may respond to confusion, fear, or physical discomfort with behaviors that appear harmful or aggressive, even toward themselves. Recognizing this as a potential manifestation of the disease can help you respond with empathy instead of panic.
Why Do People With Dementia Sometimes Hurt Themselves?
If you’ve witnessed a loved one with dementia engaging in self-harming behavior, you’re likely desperate for answers. It’s a deeply unsettling experience, especially when the person can’t explain why they’re doing it. Understanding the why behind these actions is the first step in shifting your response from fear to informed support.
Self-injury in people with dementia can result from a complex mix of neurological, emotional, and psychological factors. Here’s what you need to know:
1. Brain Changes That Affect Impulse Control and Pain Perception
Dementia alters how the brain processes information and regulates behavior. Damage to areas responsible for judgment, self-awareness, and impulse control, such as the frontal lobe, can lead someone to act out in ways that may seem erratic or even harmful. In some cases, a person may not even recognize that they are hurting themselves due to altered pain perception or a delayed reaction to discomfort.
2. Confusion, Frustration, or Sensory Misinterpretation
Imagine living in a world where familiar people feel like strangers, and daily routines no longer make sense. That kind of cognitive disorientation often triggers extreme frustration, anxiety, or fear. When verbal communication fails, some people with dementia may express distress through physical means hitting themselves, pulling at their skin, or banging their heads.
In certain cases, what looks like self-harm is a response to sensory misinterpretation. For example, someone may scratch aggressively at their skin because they believe something is crawling on them. These perceptual distortions can be symptoms of advanced dementia, including Lewy Body or Alzheimer’s.
3. Co-Existing Mental Health Conditions
It’s also important to consider overlapping psychiatric conditions. Many people with dementia experience depression, anxiety, psychosis, or even late-onset bipolar disorder. These mental health challenges can intensify emotional instability and increase the risk of self-destructive behaviors.
Supporting Data to Strengthen Understanding
- The Alzheimer’s Association notes that behavioral symptoms such as agitation, aggression, and restlessness are common in mid-to-late stages of dementia.
- Research from the National Institutes of Health (NIH) highlights how cognitive decline often leads to disinhibited behavior, including self-injury, particularly in cases of frontotemporal dementia or advanced Alzheimer’s disease.
Recognizing these root causes can help you stop asking “why is this happening?” and start planning what you can do next. You’re not powerless, and the next section will help guide your response.
Is self-mutilation a symptom od dementia?
It’s a difficult question to ask, but one that becomes unavoidable when you begin noticing signs of self-injury in someone with cognitive decline. You might be wondering if what you’re seeing is part of the disease process or something separate altogether. So, let’s get clear: is self-mutilation a symptom of dementia?
While self-mutilation is not considered a core symptom of dementia, it can emerge as a secondary behavioral complication, especially in the later stages of the disease. As dementia progresses and cognitive functions decline, some individuals may engage in self-injurious behaviors, not out of suicidal intent, but due to confusion, physical discomfort, or a loss of impulse control. Understanding the forms this behavior can take is key to knowing how to respond effectively.
Forms of Self-Injury in Elderly Patients With Dementia
Not all self-harming behaviors look the same. In dementia, self-injury often manifests in ways that are subtle at first and gradually intensify. Here are the most common presentations you might encounter:
• Scratching, Hitting, Biting, or Cutting
You may notice repeated scratching of the same area, unexplained bruises, or even bite marks. Sometimes, these actions are attempts to relieve an imagined itch or discomfort. In other cases, they’re expressions of frustration when words fail.
• Refusal to Eat or Drink (Self-Neglect as Harm)
Although less obvious, consistent refusal to eat, drink, or take medication can be a form of passive self-harm. The person may not consciously intend to harm themselves, but their actions, or lack thereof, can have serious physical consequences.
• Repetitive Harmful Behaviors (e.g., Head-Banging or Skin-Picking)
Some dementia patients exhibit compulsive repetitive actions like banging their head against furniture, pulling their hair, or picking at their skin until it bleeds. These behaviors can stem from overstimulation, discomfort, or neurological misfiring.
These forms of self-injury don’t always fit the conventional definitions used in mental health diagnoses, but they are just as serious. Recognizing them early and understanding their root causes can help you intervene in ways that are both safe and compassionate.
Next, you’ll learn how to evaluate the severity of these actions and when they require urgent attention.
When to Be Concerned
As a caregiver or loved one, it can be difficult to know when self-injury crosses the line from occasional frustration to something more serious. Not every scratch or refusal to eat is cause for panic, but patterns matter. Paying attention to both the frequency and severity of these behaviors is essential to protect your loved one’s well-being.
1. How Often Is It Happening?
If you’re noticing repeated self-harming behavior such as daily skin-picking, biting, or hitting, that’s a clear sign something deeper is going on. Even if the actions seem minor at first, consistent repetition could indicate growing distress or a neurological trigger that needs medical evaluation.
Ask yourself:
- Is this behavior happening more often over time?
- Are the actions becoming more intense or more harmful?
- Is the person aware they’re doing it, or completely unaware?
2. What’s the Severity?
Mild scratching might not raise alarm right away, but bleeding wounds, visible bruising, or evidence of deliberate injury (like cutting or head-banging) should never be ignored. The more severe the harm, the more urgently intervention is needed both to ensure safety and to explore possible medical or psychiatric causes.
3. Could It Be a Form of Communication?
In many cases, self-injury is not just a behavior it’s a message. When verbal communication breaks down, someone with dementia may act out physically to express:
- Physical discomfort or pain
- Overwhelming fear or anxiety
- Frustration from being misunderstood
- A need for attention or connection
If the person becomes agitated in specific situations like loud environments, bathing routines, or being touched, they may be using self-harm to signal distress in the only way they can.
By watching for these patterns and triggers, you gain insight into what your loved one may be experiencing internally. These behaviors are never random. They’re signals and your awareness is the first step toward getting them the right help.
Clinical Insight: Distinguishing Between Intentional and Unintentional Harm
When you witness self-injurious behavior in someone with dementia, one of the most difficult questions you’ll face is this: Are they doing this on purpose, or is it something they can’t control? Understanding the difference between intentional and unintentional self-harm is crucial for determining the right care path.

Accidental vs. Deliberate Behavior in Dementia
In dementia, the line between voluntary and involuntary actions often becomes blurred. A person might repeatedly injure themselves without fully realizing it, or they may believe they’re doing something necessary or helpful, even if it’s harmful.
Here’s how you can start to distinguish between the two:
- Unintentional Harm:
- The person seems unaware of their actions
- Injuries occur during repetitive behaviors (e.g., rubbing skin raw, hitting an object without restraint)
- There’s no expressed emotional reasoning behind the act
- Intentional Harm:
- The person acknowledges pain or emotional distress
- There’s a visible emotional trigger (e.g., anger, sadness, paranoia) before the behavior begins
- Harm appears calculated or targeted (e.g., cutting specific areas, refusing all food as a form of protest)
That said, intentional doesn’t always mean suicidal in dementia, deliberate self-harm can be a symptom of other underlying conditions.
Psychiatric Comorbidities Can Play a Role
It’s not uncommon for people with dementia to also suffer from mental health disorders, especially in the middle and later stages. Depression, anxiety, psychosis, and even late-onset bipolar disorder can all increase the risk of self-injurious actions.
Here are some psychiatric conditions to watch for:
- Depression may manifest as self-neglect, loss of the will to eat, or refusal of basic care.
- Psychosis: The person may respond to delusions or hallucinations by harming themselves.
- Agitated Delirium: Common in hospital settings, this can involve aggressive or harmful behavior.
- Frontal Lobe Dementia (FTD): Known for impulsive, socially inappropriate, or harmful actions due to executive function breakdown.
If you’re unsure whether what you’re seeing is deliberate or a symptom of cognitive decline, consult a neurologist, geriatric psychiatrist, or behavioral specialist. With professional insight, you can get a clearer picture and ensure your loved one gets the care they deserve.
Self-Harm Treatment Centers: Are They Suitable for Dementia Patients?
If you’re considering professional help for a loved one with dementia who is engaging in self-harm, you might be wondering whether typical self-harm treatment centers are the right option. The truth is, not all treatment centers are created equal, and the needs of someone with dementia can be very different from younger individuals who self-injure.
Specialized vs. General Mental Health Facilities
When looking for treatment centers, it’s important to understand the distinction between geriatric psychiatric units and general or youth-focused self-harm centers:
- Geriatric Psychiatric Units
These facilities specialize in the unique mental health needs of older adults, including those with dementia. Staff here are trained to handle cognitive impairments, manage dementia-related behaviors, and address co-existing medical conditions. They provide tailored interventions that focus on safety, emotional support, and cognitive stabilization. - Youth-Focused Self-Harm Centers
Many self-harm treatment centers are designed primarily for adolescents and young adults struggling with self-injury related to trauma, depression, or personality disorders. While they offer excellent care for that population, their approaches may not be suitable or even safe for elderly patients with dementia.
What This Means for You
If you’re seeking a treatment center for someone with dementia, prioritize geriatric psychiatry programs or memory care units that incorporate behavioral health services. These centers understand the cognitive challenges your loved one faces and can adapt therapies accordingly.
Look for facilities that offer:
- Staff trained in dementia care and geriatric psychiatry
- Multidisciplinary teams including neurologists, psychologists, and social workers
- Behavioral interventions tailored to dementia-related symptoms
- Environment designed for the safety and comfort of elderly patients
Choosing the right care setting can make a significant difference in managing self-harm behaviors safely and compassionately. You deserve peace of mind knowing your loved one is in capable hands.
What to Expect in a Treatment Program
If you decide to explore professional help for dementia-related self-harm behaviors, it’s natural to wonder what treatment will look like. Understanding the typical components of a treatment program designed for dementia patients can help you feel more confident as you navigate this process.
1. Comprehensive Assessment Protocols
When you bring your loved one to a specialized treatment center or geriatric psychiatric unit, the first step will usually be a thorough assessment. This includes:
- Evaluating cognitive status and dementia severity
- Screening for co-existing psychiatric conditions like depression or anxiety
- Reviewing medical history and medications
- Identifying potential triggers for self-harming behavior
This comprehensive evaluation helps the care team tailor interventions specifically to your loved one’s unique needs.
2. Cognitive Therapy Adaptations
Standard cognitive behavioral therapies (CBT) may not be suitable for everyone with dementia due to memory and processing challenges. Instead, treatment programs adapt these therapies by:
- Using simple, repetitive techniques to reinforce positive behaviors
- Incorporating sensory-based activities to reduce agitation
- Focusing on emotional regulation strategies that do not rely heavily on verbal communication
You’ll find that these adapted therapies prioritize safety and emotional comfort over traditional talk therapy.
3. Medication and Behavioral Strategies
In some cases, medication may be prescribed to help manage symptoms such as anxiety, depression, or agitation that contribute to self-harm. Common approaches include:
- Low-dose antipsychotics or mood stabilizers (carefully monitored)
- Anti-anxiety medications
- Non-pharmacological methods like music therapy, aromatherapy, or structured routines to reduce distress.
Behavioral strategies focus on identifying triggers and reinforcing safer coping mechanisms. Care teams often work closely with you to maintain consistency between treatment settings and home environments.
By knowing what to expect, you can better advocate for your loved one’s care and actively participate in their journey toward stability and safety.
Choosing the Right Center
When it comes to finding a self-harm treatment center suitable for someone with dementia, you want to be sure you’re making the best choice. Not all facilities are equipped to handle the unique challenges dementia presents, so here’s a straightforward checklist to guide your decision:
Checklist: What to Look For in a Treatment Center
- Dementia-Capable Staff and Training
You want caregivers and clinicians who understand the complexities of dementia. Staff trained in cognitive decline are better equipped to recognize self-harm behaviors and respond with patience and appropriate techniques. - Geriatric Psychiatry Support
The presence of specialized geriatric psychiatrists is crucial. They can provide expert diagnosis, medication management, and tailored therapy plans designed for older adults with overlapping mental health concerns. - Trauma-Informed Care Approaches
Self-harm often signals deeper emotional pain or trauma. Centers that practice trauma-informed care prioritize safety, trust, and empowerment, helping your loved one heal without re-traumatization.
By ensuring the treatment center meets these standards, you increase the chances your loved one will receive compassionate, effective care tailored to their specific needs. This careful choice can make a lasting difference in their safety and quality of life.
At-Home Interventions and Caregiver Strategies
While professional treatment centers offer specialized care, much of the day-to-day safety and comfort of someone with dementia happens at home. You play a vital role in reducing risks and supporting healthier behaviors. Here are some immediate steps you can take to protect your loved one and create a calmer environment.
Immediate Steps to Ensure Safety
1. Remove Harmful Objects
Take a careful look around your home and remove or secure items that could be used to inflict injury sharp objects, scissors, knives, or even certain household chemicals. This simple precaution can prevent accidental or intentional harm and give you peace of mind.
2. Create Soothing Routines
Consistency is your ally. Establish daily routines that provide structure and predictability, which help reduce anxiety and confusion. Incorporate calming activities like gentle music, aromatherapy, or light exercise to soothe restlessness and agitation.
3. Reduce Overstimulation and Confusion
Your loved one’s brain is already working overtime. Overstimulating environments noisy rooms, cluttered spaces, or frequent visitors, can heighten agitation and increase the risk of self-injury. Simplify their surroundings, minimize loud noises, and provide clear signage or cues to help with orientation.
By combining these immediate safety measures with professional support from self-harm treatment centers, you create a network of care that addresses both the physical and emotional needs of your loved one.
Long-Term Approaches
Taking care of someone with dementia who may engage in self-harm requires patience, planning, and ongoing support. Beyond immediate safety, you’ll want to focus on strategies that promote stability, emotional well-being, and collaboration with healthcare professionals over time.
1. Consistency in Daily Structure
You’ll find that maintaining a predictable daily routine is one of the most effective ways to reduce anxiety and confusion. Regular meal times, consistent sleep schedules, and familiar activities help your loved one feel more secure. When routines are disrupted, agitation and self-injurious behaviors often increase, so your commitment to consistency is key.
2. Emotional Validation Techniques
It’s important to acknowledge what your loved one might be feeling, even if they can’t express it clearly. Using simple phrases like “I see that you’re upset,” or “It’s okay to feel scared,” can soothe emotional distress. Validating their feelings rather than dismissing or correcting them helps reduce frustration and may lessen harmful behaviors.
3. Collaborating with Medical Professionals
You don’t have to do this alone. Building a strong partnership with neurologists, geriatric psychiatrists, therapists, and social workers ensures your loved one’s care is comprehensive and responsive. Share observations about self-harm behaviors, triggers, and progress regularly so the team can adjust treatment plans as needed.
By integrating these long-term approaches into daily life, you’re creating a supportive environment that addresses both the behavioral and emotional challenges linked to dementia-related self-harm.
Behavior Triggers and Suggested Responses
Understanding what triggers self-harming or agitated behaviors in someone with dementia is crucial to managing those moments effectively. Here’s a quick reference table to help you identify common triggers and how you can respond to keep your loved one calm and safe:
| Trigger | Response Strategy |
|---|---|
| Loud noises | Use noise-canceling headphones or create a quiet space to reduce auditory overload. |
| Confusing environment | Simplify the décor by removing clutter and label rooms or objects clearly to aid orientation. |
| Physical discomfort | Regularly check for pain, infections, or other medical issues that could cause distress. |
| Loneliness or isolation | Introduce companionship through visits, phone calls, or interactive activities to reduce feelings of isolation. |
By paying attention to these triggers and proactively addressing them, you’re helping prevent self-harm behaviors before they start, making daily life safer and more comfortable for both of you.
Self-Harm Scar Treatment in Elderly Skin
Caring for scars caused by self-harm in someone with dementia requires special attention. You might already know that older skin is very different from younger skin, but you may not realize just how much these differences affect healing and treatment options.
Why Scar Treatment Needs Are Different in Older Adults
As you care for someone older, it’s important to understand that their skin is thinner, more fragile, and less elastic than that of younger individuals. This means:
- Slower Healing: The natural repair process takes longer, increasing the risk that wounds might reopen or become irritated.
- Increased Risk of Infection: Because the skin’s protective barrier is weaker, scars and wounds are more vulnerable to bacteria, which can lead to infections if not properly treated.
- Greater Sensitivity: Certain topical treatments or bandages that work well for younger skin might cause irritation or allergic reactions in older adults.
Given these factors, your approach to self-harm scar treatment must be gentle, patient, and closely monitored. You’ll want to avoid harsh chemicals and opt for treatments that support healing without adding stress to the skin.
Understanding these differences will help you choose the safest and most effective options to care for your loved one’s scars while minimizing discomfort and complications.
Safe Scar Treatment Options
When it comes to treating self-harm scars on elderly skin, safety and gentleness are your top priorities. You want treatments that support healing without causing irritation or additional damage. Here are some of the safest and most effective options you can consider:
1. Silicone Gel Sheets
Silicone gel sheets are widely recommended for scar management because they help keep the skin hydrated and create a protective barrier. Using these sheets regularly can reduce the appearance of scars and promote smoother skin texture. They’re gentle enough for fragile elderly skin and easy to apply.
2. Prescription Ointments
Your healthcare provider might prescribe topical ointments that contain ingredients like silicone, vitamin E, or corticosteroids to improve scar healing. These medications can reduce inflammation and help scars fade more quickly. Always follow the guidance of a dermatologist or geriatric specialist when using prescription treatments.
3. Gentle Exfoliation and Moisturization
Mild exfoliation using soft washcloths or gentle creams can help remove dead skin cells around scars, but it must be done carefully to avoid irritation. Pair this with regular moisturization using fragrance-free, hypoallergenic creams to maintain skin elasticity and comfort.
By choosing these safe scar treatment options, you help your loved one’s skin heal as smoothly and comfortably as possible, respecting the unique needs of aging skin.
When to Consult a Dermatologist
While many scars can be managed at home with gentle care, there are times when you should seek professional dermatological advice to ensure the best outcomes for your loved one’s skin.
Deep Tissue Scarring
If scars are unusually thick, deep, or painful, it’s important to have them evaluated by a dermatologist. Deep tissue scarring can sometimes affect mobility or cause discomfort, and specialized treatments such as laser therapy or corticosteroid injections may be necessary to improve function and appearance.
Keloids or Recurring Injury Areas
Keloids are raised, thickened scars that grow beyond the original injury site. They are more common in some individuals and can become a source of ongoing irritation or discomfort. Similarly, areas where self-harm recurs frequently may develop problematic scarring that requires medical intervention. A dermatologist can recommend treatment plans tailored to these conditions, helping reduce pain and improve skin health.
Knowing when to seek expert care ensures your loved one receives the safest, most effective scar treatment possible, preserving their comfort and dignity.
When to Seek Professional Help
Knowing when to seek professional help can be overwhelming, especially when self-harm behaviors appear in someone with dementia. However, recognizing urgent warning signs and accessing the right support can make all the difference in ensuring safety and appropriate care.
Warning Signs That Require Urgent Psychiatric Evaluation
You should seek immediate help if your loved one:
- Causes severe or life-threatening injuries to themselves
- Exhibits sudden, intense agitation or aggression
- Shows signs of severe depression, withdrawal, or suicidal thoughts
- Experiences hallucinations or delusions that increase self-harm risk
These signs indicate that professional intervention is necessary to prevent harm and stabilize their condition.
Involving Neurologists, Psychologists, and Social Workers
Managing self-mutilation in dementia often requires a multidisciplinary approach. You’ll want to engage:
- Neurologists who specialize in dementia and cognitive disorders
- Psychologists or psychiatrists trained in geriatric mental health and behavioral therapy
- Social workers who can coordinate care plans, community resources, and caregiver support
Working with this team ensures your loved one receives comprehensive treatment tailored to both their medical and emotional needs.
Using Crisis Lines and Emergency Dementia Services
In moments of crisis, don’t hesitate to reach out for immediate assistance. Many regions offer 24/7 crisis hotlines specifically for dementia-related emergencies or mental health crises. Emergency dementia services can provide rapid evaluation and temporary stabilization in a safe environment.
By recognizing these critical moments and knowing where to turn, you empower yourself to protect your loved one and access the specialized care they need.
FAQs About Self-Mutilation as a Symptom of Dementia
Is self-mutilation a common symptom of dementia?
Self-mutilation is not considered one of the primary symptoms of dementia. However, you should know that it can occur in some individuals, especially during advanced stages, due to behavioral and neurological changes affecting impulse control and emotional regulation.
What should I do if my parent with dementia is hurting themselves?
Your priority is ensuring their immediate safety, removing harmful objects, and monitoring them closely. Next, consult their healthcare provider for a thorough evaluation. A mental health assessment may be necessary to address underlying causes and develop a treatment plan.
Are self-harm treatment centers appropriate for elderly patients with dementia?
Yes, self-harm treatment centers can be helpful, but it’s crucial that they specialize in geriatric care and understand dementia-related behaviors. Facilities with trained staff and tailored interventions provide the safest and most effective support.
What are the best options for self-harm scar treatment in older adults?
For elderly skin, you want gentle yet effective treatments. Silicone-based products, mild moisturizers, and regular medical consultations are among the safest options to promote healing and reduce scarring without irritation.
Conclusion: Compassion Over Judgment
Living with dementia is already a deeply disorienting and challenging experience for both your loved one and you. When self-harm behaviors appear, it can feel overwhelming, confusing, and heartbreaking. But it’s important to remember that these behaviors are often signals of distress, not willful actions.
There is support available, there is hope, and there is a path forward. Whether you’re searching for understanding, exploring care options, or seeking guidance on treatment, including self-harm treatment centers and scar care, you don’t have to face this alone.
By approaching this journey with compassion rather than judgment, you create a safer, more loving environment where healing and comfort become possible. You are stronger than you realize, and your care truly makes a difference.







